Table of Content
HHAs attest as to whether they considered equity-focused factors in the hiring of HHA senior leadership, including chief executives and board of trustees, in the applicable reporting year. HHAs report on any attempts to measure input they solicit from patients and caregivers about care disparities they may experience as well as recommendations or suggestions for improvement. Early on, privacy concerns were raised by HHAs around the collection of all-payer data and the release of personal health information. As we indicated in the study, any new collection requirements such as this typically raise concerns and OASIS was no exception. In response to the privacy concerns, CMS took steps to mask the personal health information before the data was transmitted to the Quality Improvement and Evaluation System . In the study, we collected information from HHAs and the industry including the surveying of Agencies by one of the trade organizations and note that the privacy concerns initially raised were not raised as an ongoing concern.

For CY 2023, we proposed to use the same methodology used to establish the comorbidity subgroups to update the comorbidity subgroups using CY 2021 home health data. Although it is not our intent to review all ICD-10-CM diagnosis codes each year, we recognize that occasionally some ICD-10-CM diagnosis codes may require changes to their assigned clinical group and/or comorbidity subgroup. For example, there may be an update to the MCE unacceptable principal diagnosis list, or we receive public comments from interested parties requesting specific changes.
G. Request for Information: Health Equity in the HH QRP
Dallas-based Axxess is a home health technology company that provides agencies with cloud-based software solutions. To determine the visit threshold, select the appropriate year for your date of service and HIPPS code. ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose.
Section 1895 of the Act allows for the provision of an addition or adjustment to the home health payment amount otherwise made in the case of outliers because of unusual variations in the type or amount of medically necessary care. Under the HH PPS and the previous unit of payment (that is, 60-day episodes), outlier payments were made for 60-day episodes whose estimated costs exceed a threshold amount for each HHRG. The episode's estimated cost was established as the sum of the national wage-adjusted per visit payment amounts delivered during the episode. The outlier threshold for each case-mix group or PEP adjustment defined as the 60-day episode payment or PEP adjustment for that group plus a fixed-dollar loss amount. For the purposes of the HH PPS, the FDL amount is calculated by multiplying the home health FDL ratio by a case's wage-adjusted national, standardized 60-day episode payment rate, which yields an FDL dollar amount for the case.
Resumption of Care
More recently in an article in April 2022, it was estimated that nearly half of HHAs had planned to decrease therapy utilization after the implementation of the PDGM. In the CY 2019 HH PPS final rule with comment period , we finalized a policy to maintain the current methodology for payment of high-cost outliers upon implementation of PDGM beginning in CY 2020 and calculated payment for high-cost outliers based upon 30-day period of care. Upon implementation of the PDGM and 30-day unit of payment, we finalized the FDL ratio of 0.56 for 30-day periods of care in CY 2020. Given that CY 2020 was the first year of the PDGM and the change to a 30-day unit of payment, we finalized to maintain the same FDL ratio of 0.56 in CY 2021 as we did not have sufficient CY 2020 data at the time of CY 2021 rulemaking to proposed a change to the FDL ratio for CY 2021.

With a loss-sharing ratio of 0.80, Medicare pays 80 percent of the additional estimated costs that exceed the outlier threshold amount. Using CY 2021 claims data and given the statutory requirement that total outlier payments do not exceed 2.5 percent of the total payments estimated to be made under the HH PPS, we proposed an FDL ratio of 0.44 for CY 2023. We noted that we would update the FDL, if needed, in the final rule once we have more complete CY 2021 claims data.
Table F1—U.S. Bureau of Labor Statistics' May 2020 National Occupational Employment and Wage Estimates
Therefore, we proposed to reassign the ICD-10-CM diagnosis codes listed in Table 9 from clinical group E and clinical group A (MMTA-Other) to clinical group C . The following section proposed reassignment of 320 diagnosis codes to a different clinical group when listed as a principal diagnosis, reassignment of 37 diagnosis codes to a different comorbidity subgroup when listed as a secondary diagnosis, and the establishment of a new comorbidity subgroup for certain neurological conditions and disorders. Due to the amount of diagnosis codes proposed for reassignment this year, we posted the “CY 2023 Proposed Reassignment of ICD-10-CM Diagnosis Codes for HH PDGM Clinical Groups and Comorbidity Subgroups” supplemental file on the Home Health Prospective Payment System Regulations and Notices web page. The term itself stands for “Low Utilization Payment Adjustment,” which is a standard per-visit payment for episodes of care with a low number of visits.
We send you the information to review right up front so that you can have the best data to make the best decision. This shows that we were able to discover $667.68 of additional, otherwise unclaimed revenue in the review of this chart. The LUPA threshold did not change, but often does based on the coding and OASIS suggested change. A common situation where a LUPA can be avoided would be a patient with a foley catheter. Can other things be ordered, like sending in a home health aide to check on the patient? Foley Catheter patients also have a high reimbursement rate, so it is in the best interest of the patient and agency to make a plan that can help avoid the LUPA in the first place, and being proactive about that plan.
Listing Websites about Cms Home Health Lupa Rates
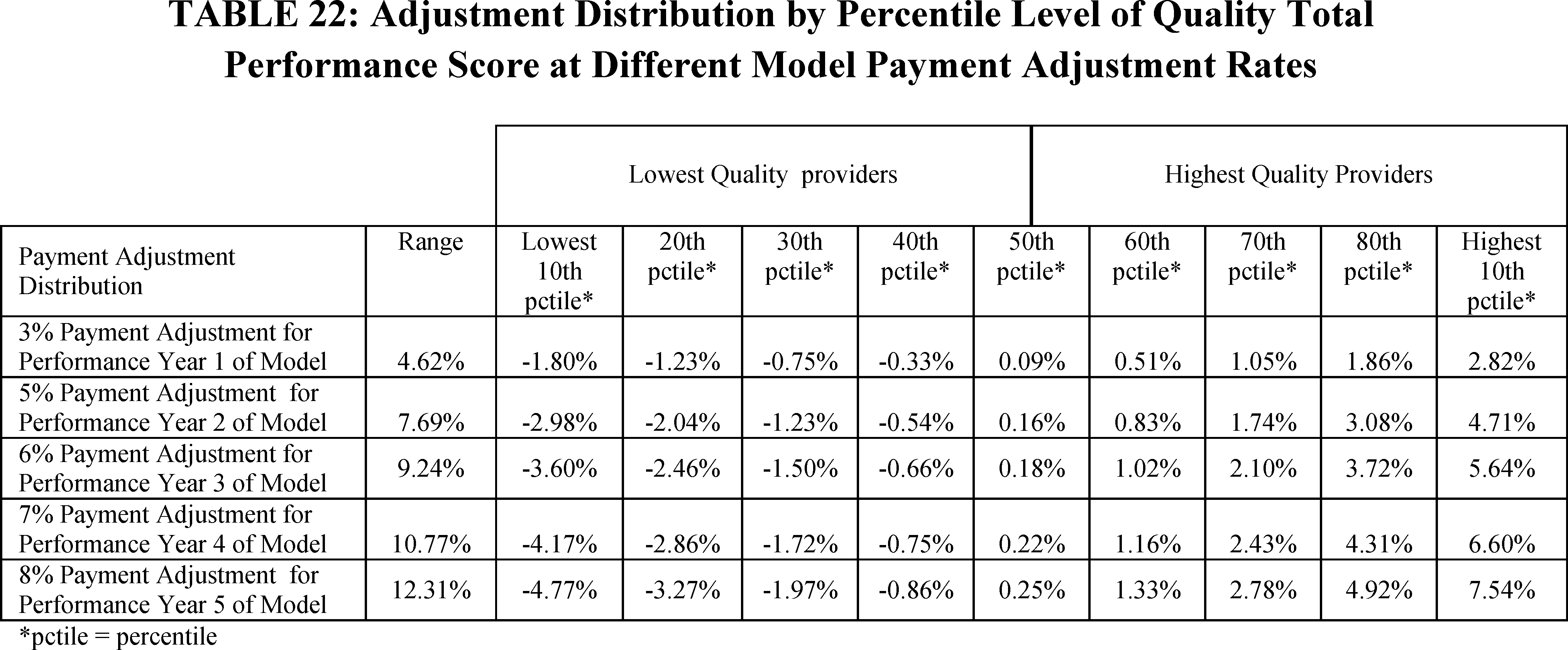
Accordingly, we proposed to change the HHA baseline year for HHAs certified prior to January 1, 2019 and for HHAs certified during January 1, 2019-December 31, 2021 for all applicable measures used in the expanded Model, from CY 2019 and 2021 respectively, to CY 2022 beginning with the CY 2023 performance year. Additionally, we proposed that for any new HHA certified on or after January 1, 2022, the HHA baseline year is the first full calendar year of services beginning after the date of Medicare certification and the first performance year is the first full calendar year following the HHA baseline year. As such, we did not calculate or propose the CY 2023 wage index as if the cap was in place for 2022. While such a policy may benefit some providers, it would change the wage index budget neutrality factor, and would impact the CY 2023 payment rates for all providers without allowing them the opportunity to comment.
However, PDGM provides an introduction towards building a better management team complex structure of visit requirement variables that Medicare home health care providers will need to navigate. Beginning on January 1, 2023, CMS applies a cap on decreases to the home health wage index such that the wage index applied to a geographic area is not less than 95 percent of the wage index applied to that geographic area in the prior calendar year. The 5-percent cap on negative wage index changes is implemented in a budget neutral manner through the use of wage index budget neutrality factors. After consideration of the public comments received, and as addressed in section III.D.
The comorbidity subgroup circulatory 10 includes ICD-10-CM diagnosis codes related to varicose veins and lymphedema. Therefore, our clinical advisors determined that Q82.0 should be assigned to the comorbidity subgroup circulatory 10 similar to other lymphedema diagnosis codes. In addition, we evaluated resource consumption related to the comorbidity subgroup circulatory 10 and Q82.0 and found no significant variations negating a reassignment. Therefore, we proposed to assign diagnosis code Q82.0 to circulatory 10 when listed as a secondary diagnosis. Our clinical advisors reviewed the 12 ICD-10-CM diagnosis codes related to crushing injury of the face, skull, and head and determined that reassignment of these codes to clinical group B is clinically appropriate because they are consistent with other diagnosis codes in clinical group B that describe injuries requiring neurological rehabilitation.
As you have seen there is a detrimental impact of on the agency hence it important to understand factors that are currently causing LUPAs with your PDGM committee. This PDGM committee should randomly review a percentage of LUPA episodes with varying diagnoses each month for the next three to four months. However, your personal and financial positions play a more critical role when becoming a homeowner. The change in length of daylight between today and tomorrow is also listed when available. The time period when the sun is between 12 and 18 degrees below the horizon at either sunrise or sunset. The sun does not contribute to the illumination of the sky before this time in the morning, or after this time in the evening.
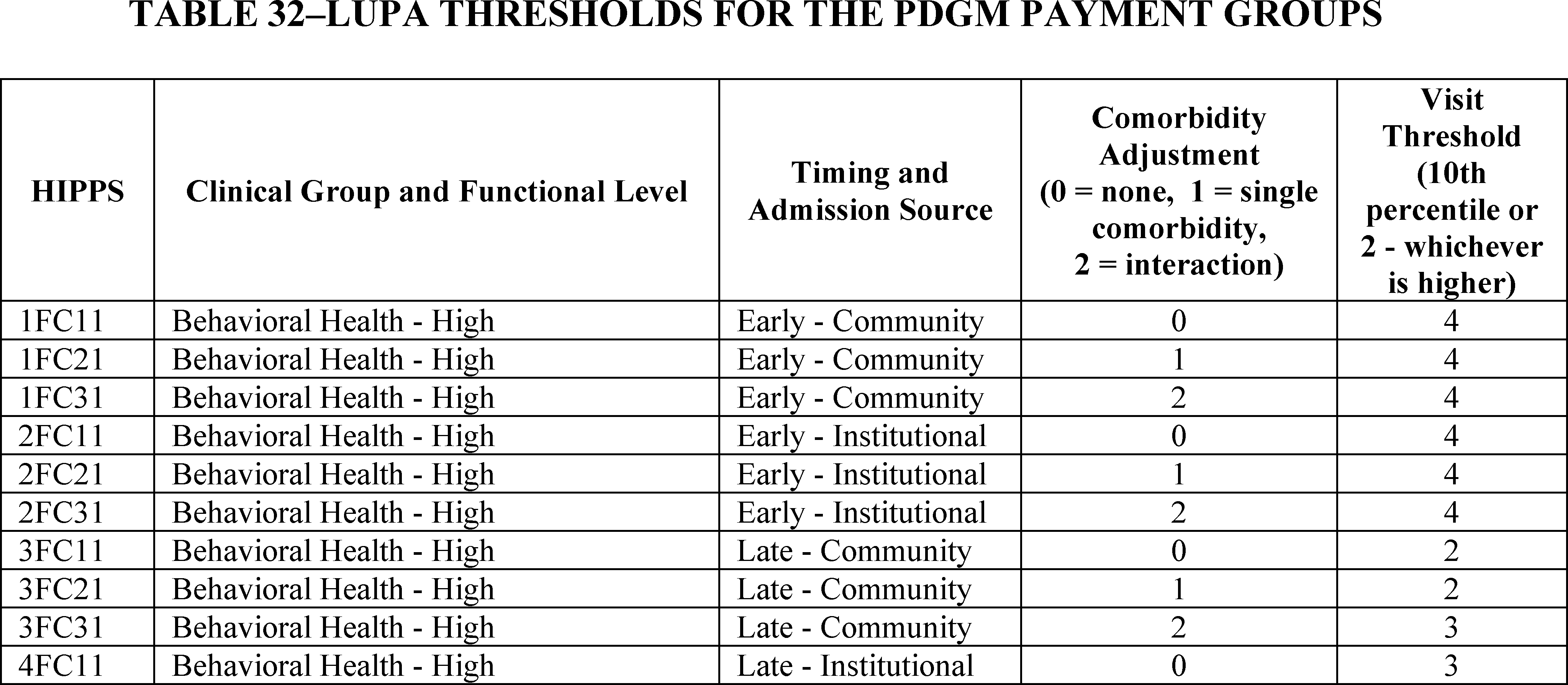
In the CY 2019 HH PPS final rule with comment period , we finalized setting the LUPA thresholds at the 10th percentile of visits or 2 visits, whichever is higher, for each payment group. This means the LUPA threshold for each 30-day period of care varies depending on the PDGM payment group to which it is assigned. If the LUPA threshold for the payment group is met under the PDGM, the 30-day period of care will be paid the full 30-day period case-mix adjusted payment amount .
As discussed in connection with our proposal to use CY 2022 data for the HHA baseline year, if we were to finalize our proposal to use CY 2022 rather than CY 2019 data for the Model baseline year, we would anticipate providing HHAs with the final achievement thresholds and benchmarks in the July 2023 IPR in the summer of CY 2023. This would be consistent with the rollout of the original HHVBP Model in which benchmarks and achievement thresholds using 2015 data were made available to HHAs during the summer of the first performance year . As set forth in the July 3, 2000 final rule , the base unit of payment under the HH PPS was a national, standardized 60-day episode payment rate.
After reviewing the CY 2021 home health claims utilization data we determined that visit patterns have stabilized. We believe that CY 2021 data will be more indicative of visit patterns in CY 2023 rather than continuing to use the LUPA thresholds derived from the CY 2018 data pre-PDGM. Therefore, we proposed to update the LUPA thresholds for CY 2023 using data from CY 2021. We reviewed Q82.0 for clinical group reassignment, as described in section II.B.3.4. During this review, we discovered Q82.0 is not currently assigned to a comorbidity subgroup when listed as a secondary diagnosis.


No comments:
Post a Comment